Coronavirus (COVID-19) Preparedness Information
Our hospital is committed to providing the highest quality care and ensuring the safety of our patients, employees, providers, volunteers and visitors. We are continuing to monitor the evolving situation with COVID-19 and are taking the necessary steps to ensure we are fully prepared to care for patients, in accordance with guidance from the Centers for Disease Control and Prevention (CDC) and in partnership with our local and state health departments.
Below are a number of resources to help educate you and your family on COVID-19. Wyoming residents with questions about COVID-19 may send an email to wdh.covid19@wyo.gov.
COVID-19 Online Risk Assessment
To help support the health of our community, we are providing access to an online COVID-19 risk assessment developed by the Centers for Disease Control and Prevention (CDC). This tool does NOT provide a diagnosis, and it should NOT be used as a substitute for an assessment made by a healthcare provider.
Quick Links:
- Centers for Disease Control and Prevention- www.cdc.gov
- Fremont County Public Health- https://www.fremontcountywy.org/government/departments/public_health/index.php
- Wyoming Department of Health – https://health.wyo.gov/publichealth/infectious-disease-epidemiology-unit/disease/novel-coronavirus/
- Fremont County Emergency Management Agency- https://www.fremontcountywy.org/government/departments/emergency_management/index.php
- Wyoming Hospital Association – https://www.wyohospitals.com/
- World Health Organization - www.who.int
SageWest Health Care is committed to protecting the health and safety of everyone who walks through our doors. We are continuing to work closely with the Wyoming Department of Health (WDH) and following guidance from the Centers for Disease Control and Prevention (CDC) to ensure the safety of our patients, the clinical team that cared for this individual and all those within our facility.
What we are doing
SageWest Health Care is committed to providing the highest quality care and ensuring the safety of our patients, employees, providers and visitors at all times. We have tested processes to respond to situations involving infectious disease year-round. Here is what we are doing to stay ready and respond to COVID-19:
- We have a robust emergency operations plan in place and are reviewing and proactively completing a number of preparation checklists out of an abundance of caution.
- We have hand hygiene products easily accessible throughout our facility.
- We are screening patients in our emergency department, inpatient units and outpatient clinics based on CDC guidance.
- Staff treating a potential COVID-19 case are provided with all appropriate personal protective equipment (PPE) to help prevent exposure.
- We have returned to our regular visitation guidelines and implemented a self-screening assessment for visitors when they enter our SageWest facilities.
As a reminder our SageWest visitation guidelines include:
- Due to room size and patient care needs the number of visitors may be limited, generally more than two visitors in a patient room are discouraged.
- Children under the age of 12 years old must be accompanied by an adult (who is not the patient) at all times.
- In the ICU, no more than two visitors per ICU patient.
- Exceptions may be made by the registered nurse caring for the patient or the nurse supervisor.
- Persons visiting patients in isolation are required to wear full PPE (gown, gloves, N95/PAPR and eye protection).
- During weekdays and regular business hours visitors should enter through the main entrance. On weekends and weekday after hours, visitors should enter through the emergency department entrance.
What you can do
It’s easy to feel helpless when faced with a barrage of news reports and social media updates regarding COVID-19. The good news is that there are some key steps you can take to help protect you and your loved ones and help prevent the spread of respiratory illnesses, including COVID-19:
- Avoiding close contact with people who are sick.
- Avoiding touching your eyes, nose and mouth.
- Staying home when you are sick.
- Covering your cough or sneeze with a tissue, then throwing the tissue in the trash.
- Cleaning and disinfecting frequently touched objects and surfaces, including your phone, computer, remote controls and doorknobs.
- Washing your hands often with soap and water for at least 20 seconds, especially after going to the bathroom, before eating and after blowing your nose, coughing or sneezing.
- Using an alcohol-based sanitizer with at least 60% alcohol if soap and water are not readily available (always wash hands with soap and water if hands are visibly dirty).
- Practicing social distancing behaviors, including working from home, avoiding public gatherings and unnecessary travel, and maintaining a distance of approximately six feet from others when possible.
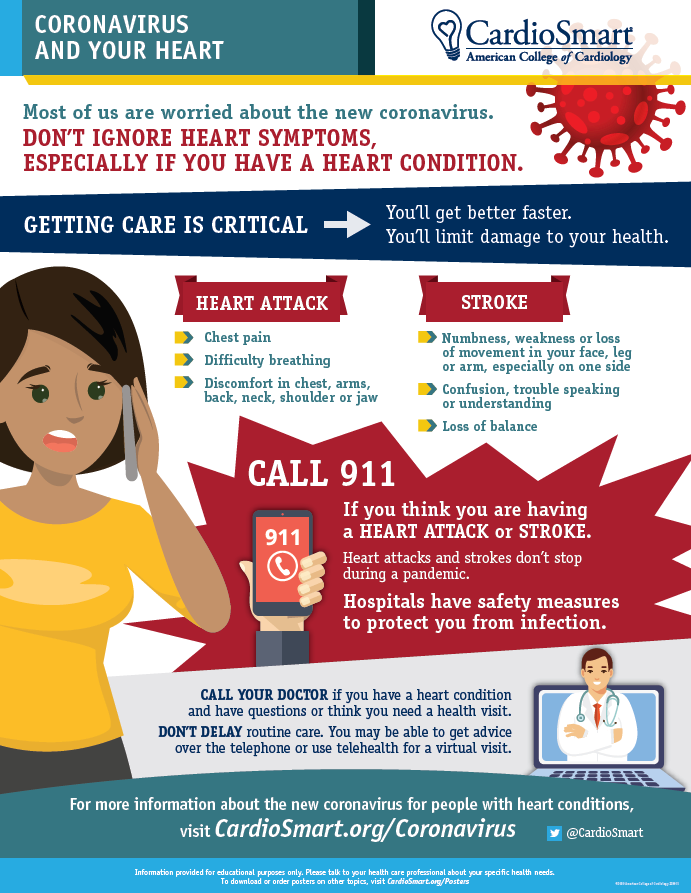
What to do if you are experiencing symptoms
First and foremost - if you are having a medical emergency, you should call 911 or go directly to the Emergency Room. If possible, notify the dispatch agent that your emergency involves symptoms possibly related to COVID-19.
For non-emergency needs, if you need medical attention due to respiratory illness symptoms (fever, cough, shortness of breath) contact your primary care provider and let them know that you are experiencing symptoms that may possibly be related to COVID-19. This will allow your provider to properly guide you and take the necessary precautions to keep others from being infected or exposed.
We want to reassure our communities that it is safe to come to the hospital should you or your family need care. Our number one priority is the health and well-being of our community – and that includes you. In collaboration with our local and state health partners we are prepared to manage an outbreak of respiratory illness, and we encourage you to follow the guidance above and stay tuned to updates from the WDH and CDC to help protect you and your loved ones. Keeping our community healthy is a community effort, and we are committed to doing everything we can to keep our community healthy. For more information and to stay abreast of the latest updates on COVID-19, you can visit SageWest Health Care SageWestHealthCare.com COVID-19 webpage and www.cdc.gov.
Wyoming 2-1-1 and the Wyoming Department of Health (WDH) are partnering to provide a public telephone helpline for COVID-19 questions and information. 2-1-1 links COVID-19 information as well as local resources and is available Monday through Friday, 8am to 6pm.
Additional Resources
Frequently Asked Questions:
Is it safe to come to the hospital?
It is safe to come to the hospital should you or your family need care, but please be mindful of our limited visitor restrictions. For the latest SageWest Health Care updates, please visit our hospital website at SageWestHealthCare.com.
Is the hospital currently limiting visitors, restricting access or on lockdown?
SageWest has returned to our regular visitation guidelines. For the latest SageWest Health Care updates, please visit our hospital website at SageWestHealthCare.com.
Should I reschedule or cancel my office visit, procedure and/or surgery?
Please consult with your doctor before cancelling or rescheduling regularly scheduled appointments and procedures.
What are the symptoms of COVID-19?
- The most common symptoms are cough, fever, shortness of breath, fatigue, sore throat, muscle aches, loss of taste or smell, nasal congestion or running nose, GI symptoms, nausea, vomiting, diarrhea, abdominal pain and headaches.
- If you are experiencing severe warning signs including difficulty breathing or shortness of breath; persistent pain or pressure in the chest; new confusion or inability to arouse; and/or bluish lips or face, call 9-1-1 immediately.
I think I’ve been exposed. What should I do if I’m experiencing symptoms?
If you develop a cough, fever or other symptoms consistent with a respiratory illness, call your doctor or our Fremont County Public Health at 332-1073 or 856-6979. If you are experiencing shortness of breath or difficulty breathing, call 9-1-1.
What happens if I’m experiencing symptoms and come to the hospital?
- First - if you can - please call ahead to your provider or the local health department. Wyoming Department of Health has a statewide helpline that provides free, confidential information and referrals to health and human services. By dialing 2-1-1, people are linked to information about COVID-19 as well as local resources, from both government and nonprofit agencies. 2-1-1 is available Monday through Friday, 8 am to 6pm. Questions can also be emailed to wdh-covid19@wyo.gov
- All patients arriving at the hospital are asked to wear a mask.
- You will be screened – and if considered high-risk based on your symptoms and/or recent travel history and potential exposure– you may be evaluated and tested in accordance with guidance from Fremont County Public Health and Wyoming Department of Health and the CDC.
What are reliable sources for information related to COVID-19?
Visit our website SageWestHealthCare.com for information on how the SageWest Health Care is preparing and for additional resources and links to reputable sources including:
- Centers For Disease Control and Prevention (CDC) – CDC.gov
- Fremont County Public Health– 332-1073 or 856-6979
- Wyoming Department of Health – 2-1-1
How can I prevent being exposed to and/or spreading COVID-19?
Visit the CDC’s website at cdc.gov or consult Fremont County Public Health and Wyoming Department of Health to learn more. SageWest Health Care also provides links to these pages on our hospital website SageWestHealthCare.com.
Frequently Asked Questions (FAQs) related to Environmental Services
Is the hospital clean and safe?
Our hospital is clean and safe – just like it always has been! One of the core elements of properly managing infectious diseases is the cleanliness of our physical facility. We follow the latest guidelines from the Centers for Disease Control and Prevention (CDC) regarding cleaning and disinfecting protocols to ensure the health and safety of everyone who enters the facility.
What specific steps are you taking to maintain a clean and safe environment?
- We comply with best practices for infection prevention of infectious diseases like COVID-19, which include:
- following hand hygiene protocol and utilizing appropriate personal protective equipment (PPE) at all times
- ensuring availability and access to hand sanitizer and soap throughout the facility
- using proper disinfectants, cleaning agents and supplies that meet state and federal infection control standards
- Our teams conduct terminal cleaning and disinfection of all sterile areas, including operating and procedural rooms, in accordance with industry standards and best practices.
- We have enhanced cleaning and disinfection of high-touch items and surfaces in high-traffic areas of our facility, including our emergency room, lobbies, waiting areas, hallways, restrooms, elevators.
- Inspections and rounding have been increased to monitor compliance of our multi-step cleaning and disinfection process.
In addition to reinforcing our routine cleaning techniques, we are also educating and training our teams on the latest guidance and recommendations for infection prevention related to COVID-19.
COVID-19 Testing Frequently Asked Questions
How do I get tested for COVID-19?
At this time, tests for COVID-19 require a provider order. Visiting a provider does not necessarily mean you need testing or that you will receive testing. Your provider will work with Fremont County Public Health to follow all appropriate guidelines from the Centers for Disease Control and Prevention (CDC) and Wyoming Department of Health to determine if testing is recommended based on your symptoms, exposure and recent travel history.
What are the qualifications for being tested for COVID-19?
Someone may be a candidate for testing if he or she has:
- A fever and cough or shortness of breath AND has been in close contact with a laboratory-confirmed COVID-19 case; or
- A fever and cough or shortness of breath and a history of travel from affected geographic areas; or
- A fever and cough or shortness of breath requiring hospitalization with no other source of infection.
Can I pick up or buy a test kit for COVID-19?
Not currently available at SageWest.
What do I do if I’ve been exposed to someone with a confirmed case of COVID-19? I want to be tested.
If you have been exposed to someone with a confirmed case of COVID-19, you should self-monitor for fever or symptoms of respiratory illness for 14 days. If you begin to experience fever or symptoms of respiratory illness, and they are mild enough that you can manage them at home, you should remain at home in isolation. Fremont County Public Health has requested if you are in self-isolation please call 857-3677 or 856-6979 to talk to a public health nurse. For details about how to correctly perform home isolation, tips for managing your illness at home with family members, and guidance on when you can discontinue home isolation, please visit the CDC’s website (link to: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html#:~:text=If%20you%20do%20not%20have,more%20reliable%20negative%20test%20result.)
If you are not experiencing symptoms, or you are experiencing mild symptoms you can manage at home in isolation, you do not need to seek medical care or testing.
I believe I have symptoms of COVID-19. What do I do next?
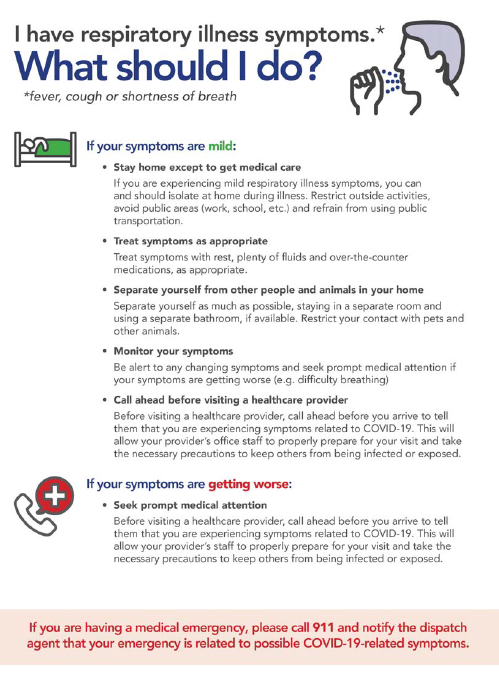
I’m experiencing mild symptoms right now, but I’m worried.
If you are experiencing fever and/or mild symptoms of respiratory illness, you can and should isolate at home during illness. For details about how to correctly perform home isolation, tips for managing your illness at home with family members, and guidance on when you can discontinue home isolation, please visit the CDC’s website (link to: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html)
Should I get tested? Isolating yourself at home and self-monitoring mild symptoms is the best course of action unless you feel you need medical care.
Worsening symptoms – I need to see my provider.
Be alert to any changing symptoms and seek prompt medical attention if your symptoms are getting worse. If you feel you need to visit your healthcare provider, call ahead before you arrive to tell them you’re experiencing symptoms that may be related to COVID-19. This will allow your provider’s office staff to properly prepare for your visit and take the necessary precautions to keep others from being infected or exposed.
Will I be tested? Your provider will make this determination based on your symptoms, and recent travel history. You may or may not be tested, but your provider will follow all appropriate CDC and Wyoming Department of Health guidelines.
Emergent symptoms – I am having difficulty breathing.
If you are experiencing a medical emergency, please call 9-1-1 and notify the dispatch agent that your emergency is related to possible COVID-19 symptoms.
Will I be tested? Your emergency medicine provider will make this determination based on your symptoms and recent travel history. You may or may not be tested, but your provider will follow all appropriate CDC and Wyoming Department of Health guidelines.